This week, week 4 post op and PWB seemed to start out on decent footing, pun intended. That is until yesterday happened when my family and I spent 8 hours at the hospital, 5 of which were in the lovely ER.
I had been noticing some odd ropy swelling near and below my calf on the surgical side for a few days. But I was in the boot, splint, and casts so often the past 7 weeks that I wasn’t paying close enough attention. At first I thought it was “normal” fallout from allowing some nice guy to cut me with a knife and fix my shredded tendon. I had a little bit of pain in the calf, but I thought that was holdover from the two weeks unpleasant surgical splint which had a pokey edge at that spot. It finally dawned on me that I should check this out. One phone call to the triage nurse with me uttering the magic words: “I have some pain in my calf.”
With a slightly panicky sound in her voice the triage nurse informs me that I need to immediately get into the office for an ultrasound and evaluation. After a flurry of phone calls and some logistical help from my wife, we manage to get set up for scanning at the closer by facility that my surgeon is associated with. It’s nearing the end of the work day, so my wife hustles down to my work office, picks me up, and whisks me to the hospital. That’s the last time of the day that anything happens fast. After a long two or three hours waiting for ultrasound, the painless but ticklish procedure, and the consult of ultrasound guy with my Doctor, the ultrasound tech comes out and informs me I need to head over to ER. It’s about this time that my blood pressure starts rising.
“ER?” I say. Why is that — did you detect something? The Ultrasound tech mumbles something under his breath about needing a doctor to evaluate the results. Since it is already 6pm, and my surgeon has headed home, and the hospital day doctors have cleared out, the only doctor available is one in ER. The guy hands me a form as we arrive at ER and tells me to give it to the check-in gal. I am thinking, oh oh, this does not sound good. I look at the sheet of paper and there are three neat little check marks next to “DVT” line items.
ER is crowded. It’s a pretty good sized area, with a waiting room, and various examining rooms, hallways, and waiting rooms. It seems as if every room has people, multiple people it them. Family members, patients, etc. And the hallways are lined with hospital beds with several patients lying in them, waiting. Waiting for what I don’t know but my blood pressure rises some more.
After checking in I notice that the floor around the check-in desk is unusually slippery. I am in a wheelchair so no concern of falling or damaging my precious newly fixed tendon, but my hiking shoe and boot glide seamlessly over the surface as I push away from the desk. I have trouble getting the wheelchair to back up my feet are sliding so much. I mention this to the check-in nurses and they laugh and say, “Yeah, somebody else mentioned that too.” At this point my thoughts turn a bit towards the nasty with ideas like this running through my head: “Duh lady! Somebody old, and or infirmed might take a spill while checking in. Do you and the ER want to be sued?”
At this point I realize I have not peed in hours and desperately need the restroom. There is a huge guy in a hospital bed in the corridor completely blocking the restroom door. He gets moved for me, and I crutch into the restroom. It’s small and difficult to navigate, a bit dirty. I suddenly realize that we are in the “3rd world” part of the hospital.
More time passes and finally a qualified nurse brings me over for some questioning and vitals. She must feel relaxed around me, why I don’t know because I was pretty agitated, but she starts to complain about how far in outlying towns people were coming to be at that hospital. I suggested to her that maybe the people in ER had their regular doctors there, or like me had moved around a bit further and further afield to find affordable housing, but had kept their primary at the hospital. This did not placate her. In any event she took my blood pressure: 155/105. Now I know that’s a bit high, and if this had been 3 years ago I wouldn’t have thought too much about it since I do, or did have high blood pressure. But with my recent health and nutrition kick, losing some weight, dropping the alcohol (mostly, but not completely), ditching cigar use, I had managed to get my blood pressure down to a normal range of 120/80 confirmed by multiple tests and devices. So now I am looking unahappily at the numbers. She informs me that I probably do have a clot, and that hopefully I will be released with medication and not have to spend the night. Sigh. The blood pressure ticks up.
Unbeknownst to me it turns out that once you are in the ER (at least at my hospital) they are required to take your vitals every hour. So apparently after an hour (but if feels less) another nurse tech comes over. This time my blood pressure rings in at 177/110. I look at the numbers and then the tech. He mutters to himself: “that can’t be.” Turns to me and says, “let’s try again.” At first I am concerned that the numbers are going to only go up forcing them to go into some sort of emergency life-saving mode. I take a deep breath, and luckily the readings drop to 155/110.
Much more time passes. Some blood is drawn to “save time.” My wife and kid head to the cafeteria before it closes. More time passes. At some point I get tired of being in the wheelchair, get on my crutches and start heading for a padded chair. As I crutch by the check-in desk it happens: FLAM! My crutch hits the super-buffed-more-slippery-than-ice waiting room floor. I head down for a crash. Ah ha! But fall down, not me. I have two feet. Unfortunately one of them is the foot with my achilles repair, but this all happens in a flash. I plant my bad foot (luckily in Aircast boot) down hard. Pain surges into my foot and up my leg. F***K I exclaim. I manage to keep from crashing down. After regaining my balance and a kindly gentleman helping I GLIIIDE into a chair. I angrily look at the check in nurse and say: “Maam! I almost fell. Do something about that ungodly slippery floor already.” I check my Achilles and as far as I can tell: no re-rupture. Phew.
The wife and kid return and I angrily describe the incident. After a little while I go back to the desk and ask the gal if she’s called anybody. I calmly explain to her that if I fall and re-rupture my Achilles, I am suing the ER. She informs me that she has indeed called somebody, twice. Nobody ever arrives to de-slick that floor.
Finally I am wheeled in to the swipe-badge only part of ER where the real action is, and lots of beds filled with people. More time. Finally the ER Doctor comes over and confirms it’s a clot. Informs me of my options: Take anti-coagulant medication, or not. But really the “not” option is not an option, so I recommend you take the medication, since that’s your only choice other than very bad things happening. Choose between a) Cumadin, or b) the newer fangled Xarelto. At first I was going to go with the more well known Cumadin because of it’s better known ability to be reverted, in the event that I were to get in accident or internally bleed and therefore need to get my blood coagulating again. But we end up opting for the Xarelto because it requires less (none really) monitoring, thereby potentially saving my wife several extra trips driving me in the car every other day to have my Cumadin levels analyzed.
Another hour in the ER and finally the medication and prescription is actually delivered. The pill is about the size of 1/4 of a pea. I am now “laughing” inside. Eight hours for a tiny pill.
So now it is one day later and I have only taken three doses. So far no nasty side effects, but I am only at the very beginning and I am told that I might have to take this stuff for six months!
Anybody else on Xarelto?
![]()
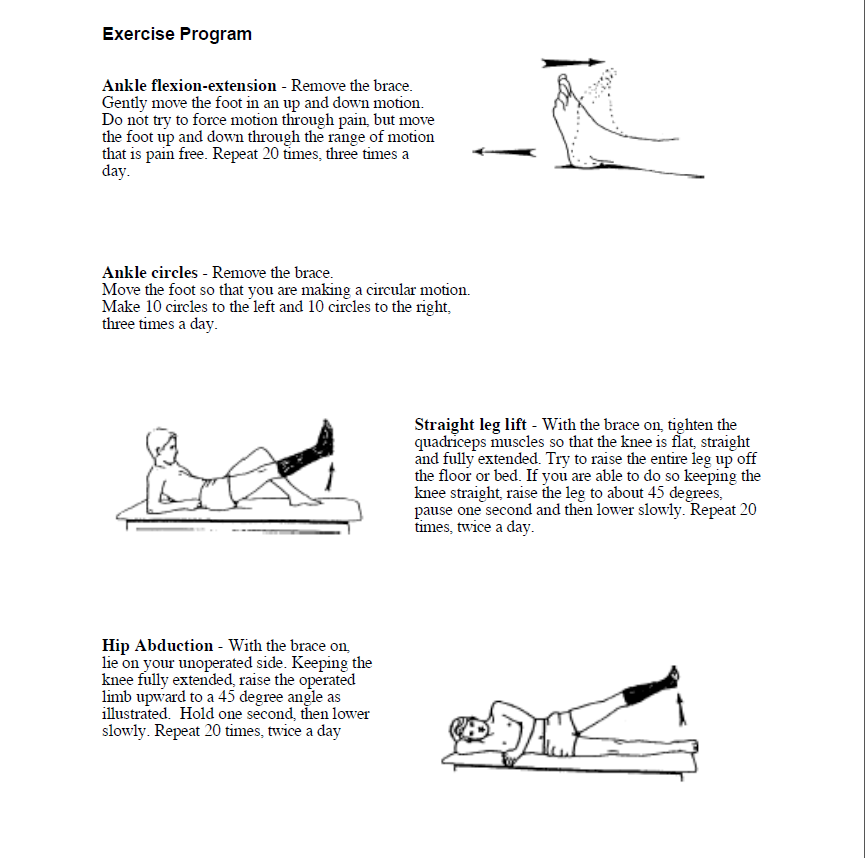
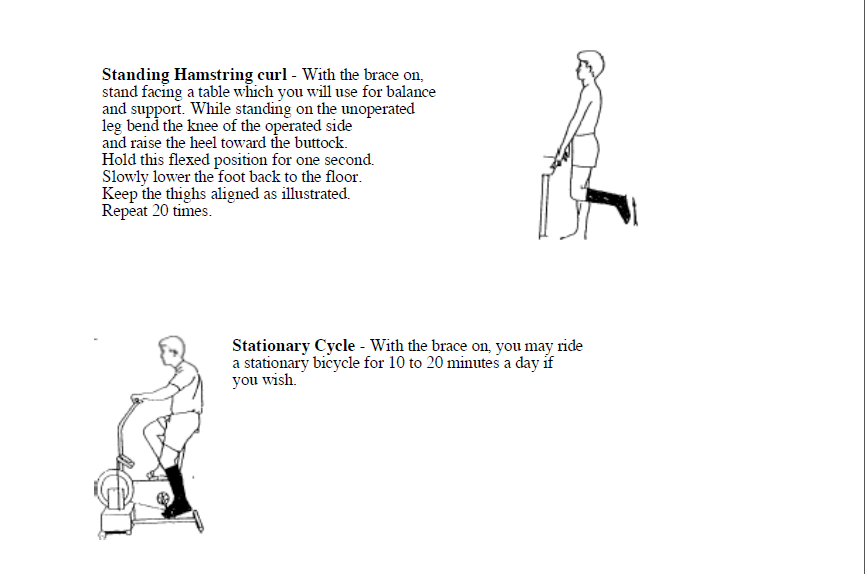
![]() I am mystified by that advice. Somebody, please clue me in as to why I am ok to put 90 pounds of force on my leg, albeit protected by a nice sturdy high-tech plastic boot, in a downward motion with thrusting force that sometimes ends in a stomp. And yet I should avoid sitting pleasantly on an indoor exercise bike and pedal for a few minutes? Oh come on get real people. Ok, enough complaining I’ll get that answer later today, time to move on.
I am mystified by that advice. Somebody, please clue me in as to why I am ok to put 90 pounds of force on my leg, albeit protected by a nice sturdy high-tech plastic boot, in a downward motion with thrusting force that sometimes ends in a stomp. And yet I should avoid sitting pleasantly on an indoor exercise bike and pedal for a few minutes? Oh come on get real people. Ok, enough complaining I’ll get that answer later today, time to move on.